Download our PowerPoint presentation by clicking here.
Approximately 15% of couples attempting their first pregnancy meet a failure. Most authorities define these patients as primarily infertile if they have been unable to achieve a pregnancy after one year of unprotected intercourse.
Conception normally is achieved within twelve months in 80-85% of couples who use no contraceptive measures, and persons presenting after this time should therefore be regarded as possibly infertile and should be evaluated.
Data available over the past twenty years reveal that in approximately 30% of cases pathology is found in the man alone, and in another 20% both the man and woman are showing reduced fertility. Therefore, the male factor is at least partly responsible in about 50% of infertile couples.
Male infertility may be various in origin. First of all we make a difference between infertility and reduced fertility. Infertility can be classified as follows:
In such cases remedies for infertility may be note easy or even being impossible to cure.
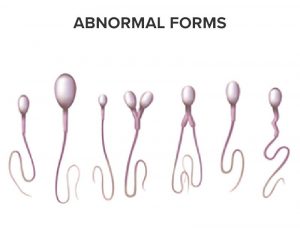
Reduced fertility on the other hand has different causes and will mostly reflect in decreased mobility of spermatozoids, malformations, reduced sperm count and other factors causing decrease of semen quality. Such factors may be:
Contact with toxic agents which may be gonadotoxic or antispermatogenic. There exist a lot of such substances with which we daily may have contact, professional or in our all-day life. These substances affect a significant proportion of the population.
Tobacco and smoking causes a harmful effect on the number, mobility and morphology of the spermatozoa by adversely affecting spermatogenesis. Furthermore, cigarette smoke is the source of the creation of activated oxygenated substances (free radicals) which are also harmful to spermatozoa.
Currently there is also an increase in the consumption of socalled recreational drugs (marijuana, cocaine).
Chronic alcohol consumption causes a reduction in the count and number of normal spermatozoa. In the case of alcoholism, sexual function is also adversely affected.
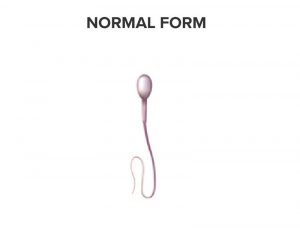
NORMAL AND ABNORMAL MORPHOLOGY - FORMS
Pharmacological agents affect fertility according to the dose used and the period over which they are prescribed.
Physical gonadotoxic events may affect us to a greater extent as they involve a large proportion of the male sex (for example: an increase in temperature in the scrotum). This may due to wearing tight clothes (jeans for instance) but also remaining seated for many hours (office work, bus, truck andtaxi drivers, long airplane flights etc.).
In order to determine the biological criteria which define a man’s fertility status, the WHO (World Health Organisation) has drawn up standards for analysing sperm.
WHO CLASSIFICATION OF “NORMAL” SEMEN PARAMETERS:
| Volume of sperm per ejaculation | 2ml |
| Concentration of spermatozoa | 20 millions / ml |
| Mobility of spermatozoa | 50% |
| Speed of progression of spermatozoa (on a scale of 0 to 4) | 3 |
| % of spermatozoa with normal morphology (WHO value) | 30% |
| Total number of spermatozoa | 40 millions |
| Total number of mobile spermatozo | 20 millions |
| Total number of functional spermatozoa | 6 millions |
Only the results of a spermogram can reveal whether there is hypofertility, normal fertility or even hyperfertility.
In cases of hypofertility confirmed by the spermogram, several nutrients have proved to be useful for improving the deficient parameters.
FERTILHOM offers a unique combination of these useful nutrients
| Nutrient composition | Daily (for 1 sachet) |
|---|---|
| L-carnitine fumarate | 2900 mg |
| Acetyl-L-carnitine | 500 mg |
| L-arginine | 250 mg |
| Glutathione | 100 mg |
| Coenzyme Q10 | 40 mg |
| Zinc | 7,5 mg |
| Vitamin B9 | 200 µg |
| Selenium | 50 µg |
| Vitamin B12 | 2 µg |
Fertilhom composition provides useful nutrients in order to increase male fertility : L-carnitine fumarate, acetylL-carnitine, L-arginine, Glutathione, Coenzyme Q10, Zinc, Vitamin B9, Selenium, Vitamin B12.

L-carnitine fumarate and acetyl-L-carnitine are the main ingredients of FertilHom. Chemically, carnitine is related to the amino acids but is not a constituent of proteins. It serves as a transporter of fatty acids to their oxidation site so that these undergo mitochondrial 3-oxidation and thus provide the energy necessary for spermatozoid mobility.
Correlations are seen in hypofertile men between the concentration of carnitine and mobility and sperm count. A supplementation of 3 g of L-Carnitin per day for 3 to 4 months to men suffering from idiopathic asthenospermia has made it possible to increase the number of mobile spermatozoa by 10% and bring about an 8% increase in spermatozoa with rapid linear progression12-20,27,32,44-45.
Arginine is a non-essential amino acid but which is necessary for the production of high-quality sperm. The physiological production of arginine reduces with age and a supplement of arginine has proved to be effective in older men. Studies show that taking supplements for several months increases the quality and quantity of the spermatozoa8,9 and therefore fertility10,11.
Glutathione acts as an antioxidant. The glutathione enzymes peroxidase and reductase play crucial roles in combatting oxidative stress damaging the quality of the sperm. Any reduction in the levels of glutathione (GSH) during spermatogenesis is clearly linked to defects in the integrity of the membrane of the spermatozoa49-51.
Coenzyme Q10 is another liposoluble antioxidant, useful for spermatozoa morphology. Its endogenous synthesis requires the presence of vitamins C, B2, B5, B6, B9 et B12 but it reduces gradually with age after 25 years of age.
Ubiquinone is extremely concentrated in the mitochondria of the intermediate part of the spermatozoa where it has a dual function: as a powerful antioxidant AND as an intermediary of the respiratory chain. Coenzyme Q10 is therefore essential for the production of energy in the spermatozoa. It performs vital functions for the spermatozoa. Indeed their great mobility involves an enormous energy requirement. Coenzyme Q10 helps to increase the number and mobility of the spermatozoa24.
Zinc is a really essential element to the reproductive function of men. In the area of fertility, it is indispensable for testicular development, spermatogenesis, the mobility of the spermatozoa and 5-α-reductase activity (the enzyme necessary for converting testosterone into 5-α-dihydrotestosterone, a biologically active form of testosterone). A zinc deficiency as a cause of oligospermia, impotence and hypogonadism has long been known about in rodents and in man5
Apart from its well-studied function as an antioxidant, selenium plays a role in the biosynthesis of testosterone and in the formation and development of the spermatozoa.
A group of researchers has moreover identified a keratinoid selenium protein called GPX4: this structural protein is associated with the mitochondrial capsule of the spermatozoa. It makes up 50% of this capsule and thus provides the integrity required by the flagellum to ensure its mobility and stability.
Unlike the other glutathione peroxidases, GPX4 does not have any direct antioxidant action at this level. Other glutathione peroxidases take care of this. It plays a role in the structure formation and thus does not act as a catalyser of reaction25.
Several studies have reported that in men with fertility problems, their vitamin B9 and B12 statuses were deficient.1-3,17,18
Indeed, any vitamin B12 deficiency is correlated with a loss of mobility and a reduced number of spermatozoa. Also, when folic acid (vitamin B9) is administered together with zinc to hypofertile men, their sperm quality is significantly better compared with administration of either vitamin B9 or zinc alone.22,46

BIBLIOGRAPHIC REFERENCES